How could technology transform patient care?
As smart devices increasingly become a part of life, clinicians and researchers are beginning to leverage the advantages of these technologies in healthcare. The ability to both passively and unobtrusively collect patient data is opening up countless new opportunities for the management and treatment of various conditions such as atrial fibrillation (AF)1.
Here’s a quick rundown of some of the technological advancements currently being researched that could transform the treatment of patients needing anticoagulation therapy.
Mobile Health
Currently, mobile health (mHealth) tools are being researched for their utility in a huge range of areas, such as telemonitoring-based feedback and improving adherence23.
A huge area of interest is the application of mobile and wearable technology for the treatment and management of AF. A recent study evaluated the efficacy of an mHealth platform in reducing AF-related adverse events3. The platform provided various support tools including: regular bleeding risk assessments and international normalized ratio (INR) measurements.
These tools have the potential to help clinicians offer integrated care throughout the trial and facilitate guideline-based treatment recommendations. In patients taking oral anticoagulants, the bleeding risks associated with anticoagulant therapy make diagnostic testing essential.
The researchers randomised 3,324 AF patients into two groups using either the mHealth platform or receiving standard care. Upon completion, they observed lower occurrences of adverse events and rehospitalisation in the mHealth intervention group compared to standard care (1.9% vs. 6.0%, respectively; p < 0.001)3.
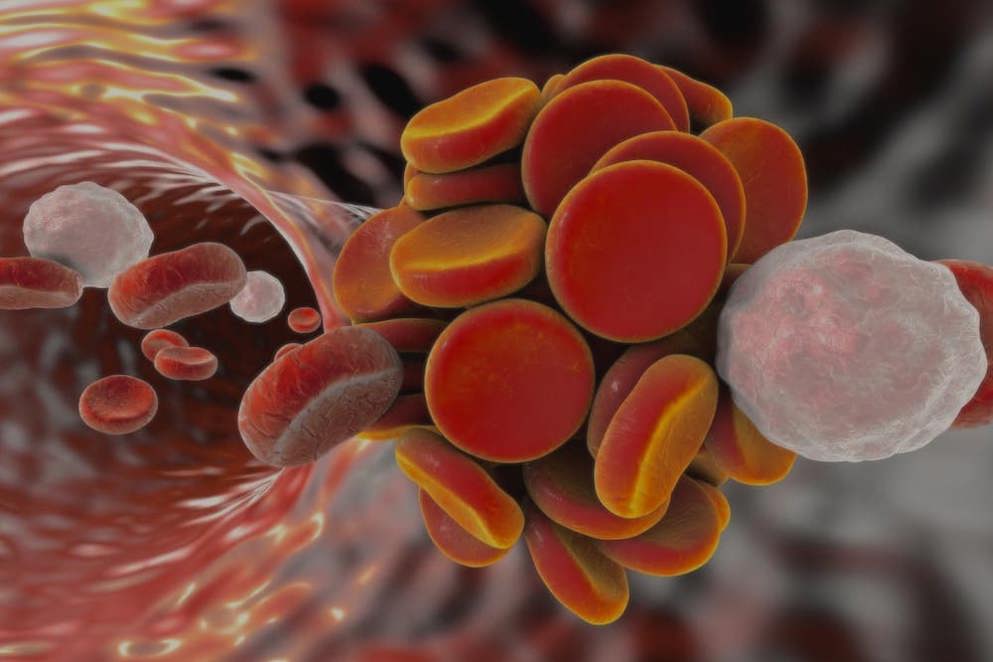
The results of this study reveal the huge potential of technology to transform the detection and treatment of AF. But if blood clots begin to form in patients with AF, could it be possible to detect them directly?
of interest
are looking at
saved
next event
3D Printing and implantable sensors
Smart implants or implantable medical devices (IMDs) have been continually developed for many years6. The latest IMDs can collect a wide range of data to aid clinical decision making and personalise diagnosis and treatment7.
An exciting new development in this field has been the recent testing of a 3-D-printed artificial blood vessel made from a material that could enable the early detection of blood clots9. Blood coagulation is a complex and tightly controlled process that results in the generation of an insoluble fibrin clot. The early detection of blood clots could be used to prevent a variety of conditions including transient ischaemic attacks.
The artificial vessel, made of a flexible composite with piezoelectric properties, can produce electric pulses based on pressure fluctuation. This allows it to detect blood pressure changes within the vessel without the need of an external power source9.
The unique 3-D geometry also allows the implant to detect if there is irregular motion caused by a blood clot within the vessel9. The detection of clots within the vessel could provide a unique method to prevent implant failure and allow for early intervention with anticoagulation.
While tested within an artificial circulatory system, further testing will be needed in vivo to determine the utility of this new material.
of interest
are looking at
saved
next event
Polymeric heart valves
As the global population continues to live longer and with more complicated medical conditions and comorbidities10, longer lasting and more effective prosthetics are essential.
Currently, patients with mechanical prosthetic valves are recommended to have anticoagulation with a VKA and INR monitoring. In patients with mechanical valves and uncontrollable bleeding, the reversal of anticoagulation using prothrombin complex concentrate (PCC) or fresh frozen plasma (FFP) is also recommended.
A new polymeric heart valve, that has the potential transform the standard treatment of patients with valvular heart disease, has recently been developed by scientists at the universities of Bristol and Cambridge11.
In vitro evaluation revealed a durability equivalent to thirty years11 and in vivo testing showed good haemodynamic and biocompatibility with no evidence of any acute valvular clot or thrombus11. These results open up the possibility of longer lasting and more biocompatible transplanted heart valves with a decreased dependence on anticoagulation.
The personalised and stratified approach to medicine that this technological advancement and others can provide has the real potential to improve how we monitor bleeding risks, inform treatment decisions and bring us closer together than ever before.
If you found this interesting, you may also enjoy learning how aPCC compares to 4-FPCC for treating warfarin-associated major haemorrhage or find other recent publications on anticoagulation and its reversal by visiting our publication digest section.
of interest
are looking at
saved
next event
of interest
are looking at
saved
next event
References
- Bussooa A, Neale S, Mercer JR. Future of smart cardiovascular implants. Sensors (Switzerland). 2018;18(7). doi:10.3390/s18072008.
- Ahmed I, Ahmad NS, Ali S, Ali S, George A, Danish HS, et al. Medication adherence apps: Review and content analysis. JMIR mHealth uHealth. 2018;6(3):e62.
- Guo Y, Lane DA, Wang L, Zhang H, Wang H, Zhang W, et al. Mobile Health Technology to Improve Care for Patients With Atrial Fibrillation. J Am Coll Cardiol. 2020;75(13):1523–1534.
- Zeballos-Palacios CL, Hargraves IG, Noseworthy PA, Branda ME, Kunneman M, Burnett B, et al. Developing a Conversation Aid to Support Shared Decision Making: Reflections on Designing Anticoagulation Choice. Mayo Clin Proc. 2019;94(4):686–696.
- Kunneman M, Branda ME, Hargraves IG, Sivly AL, Lee AT, Gorr H, et al. Assessment of Shared Decision-making for Stroke Prevention in Patients with Atrial Fibrillation: A Randomized Clinical Trial. JAMA Intern Med. 2020. doi:10.1001/jamainternmed.2020.2908.
- Fomundam L, Lin J. Design of miniaturized high frequency printed coils for wireless power transfer to biomedical implants. In: Mediterranean Microwave Symposium. 2016. IEEE Computer Society doi:10.1109/MMS.2016.7803814.
- Ferguson JE, Redish AD. Wireless communication with implanted medical devices using the conductive properties of the body. Expert Rev Med Devices. 2011;8(4):427–433.
- Bhatnagar V, Owende P. Energy harvesting for assistive and mobile applications. Energy Sci Eng. 2015;3(3):153–173.
- Li J, Long Y, Yang F, Wei H, Zhang Z, Wang Y, et al. Multifunctional Artificial Artery from Direct 3D Printing with Built‐In Ferroelectricity and Tissue‐Matching Modulus for Real‐Time Sensing and Occlusion Monitoring. Adv Funct Mater. 2020;2002868.
- Lunenfeld B, Stratton P. The clinical consequences of an ageing world and preventive strategies. Best Pract Res Clin Obstet Gynaecol. 2013;27(5):643–659.
- Stasiak JR, Serrani M, Biral E, Taylor J V., Zaman AG, Jones S, et al. Design, development, testing at ISO standards and in vivo feasibility study of a novel polymeric heart valve prosthesis . Biomater Sci. 2020;8(16):4467.
Job number: KCT16-01-0010
Developed by EPG Health for Medthority in collaboration with CSL Behring, with content provided by CSL Behring.
Not intended for Healthcare Professionals outside Europe.

