
What's wrong with Mia?
- Join Mia on her animated journey to appreciate how you can improve the lives of young people like her
- Appreciate the burden of psoriasis to help those living with its challenges
What is life like for Mia and her family?
Let’s meet our patient Mia and her family who are going to help us understand the impact of moderate to severe psoriasis for all the family.
Note: Mia is an expert-reviewed theoretical case for educational purposes only.
In this introductory animation, Mia’s worried parents take her to see a new paediatric dermatologist. Mia has continued to put on weight and become increasingly withdrawn at school and depressed and so she has been referred by her primary care physician.
Find out about the treatments that Mia has tried in the past in the next section of the Learning Zone
Keep reading to find out about the complexities of diagnosing and treating childhood psoriasis.
Psoriasis is common in children and they may need lifelong treatment
The prevalence of psoriasis in children is difficult to determine as many cases are either missed or misdiagnosed and it varies by age, gender, psoriasis definition, study design and geographical region1.
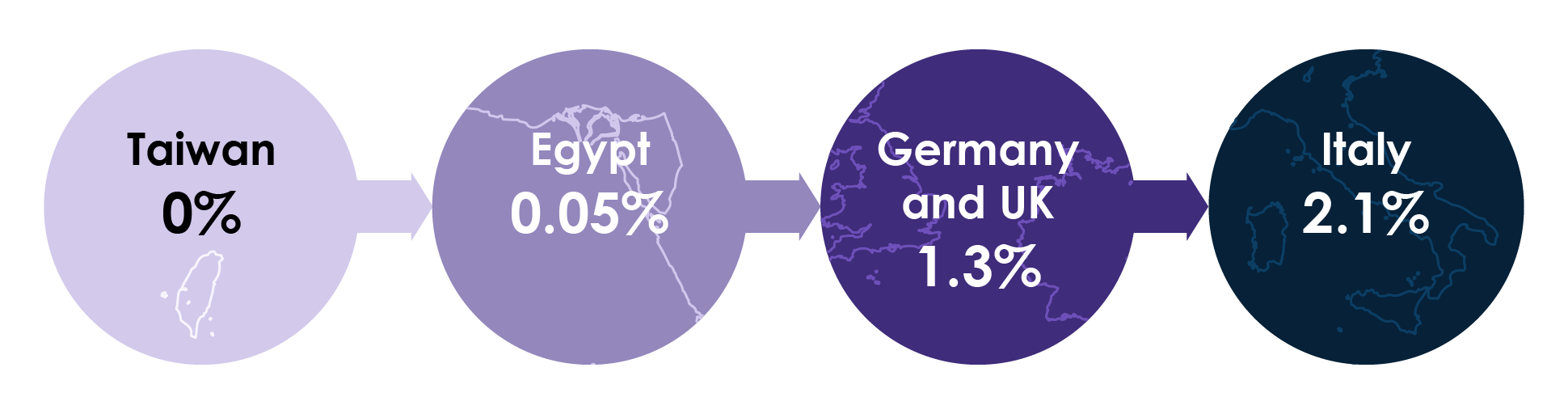
Figure 1. Range of childhood psoriasis prevalence (percentage of population) (adapted from Burden-Teh et al.2).
Around 30% of patients present with the first symptoms of psoriasis during childhood and adolescence3 and psoriasis appears more common after (0.6–1.3%) than before puberty (0.1–0.5%)2. The incidence of paediatric psoriasis is growing. Published incidence rates more than doubled between 1970–74 and 1995–991 and currently ~20,000 children under 10 are diagnosed with psoriasis every year4. With psoriasis patients making up 0.7–6.2% of the patients in paediatric dermatology clinics2, and a prevalence of 2–3% in adults3, dermatologists need to consider long-term treatment options for their paediatric patients given that psoriasis is a lifelong chronic inflammatory condition.
Indeed the paediatric psoriasis treatment paradigm appears to be shifting. Recognising the potential for lifelong symptoms and the likelihood of extracutaneous comorbidities supports a potentially more aggressive management plan in children for who a ‘less is more’ approach may not be appropriate5.
Diagnosing psoriasis and measuring QoL is more difficult in children
Diagnosis
Although the clinical subtypes of psoriasis in children are similar to adults, diagnosis in children is more challenging.
In a study of 887 patients <18 years, the most common subtypes of psoriasis were6:
- plaque psoriasis (73.7%)
- guttate psoriasis (13.7%)
- scalp psoriasis (7.6%)
- pustular psoriasis (1.1%)
Lesions in children may be thinner, softer, less scaly, less well defined than in adults7 and the clinical symptoms at presentation also vary according to the age group8. In addition, skin biopsy is performed less often in younger patients compounding the difficulty9.
Professor Vakirlis describes the dermatoscopic findings that define childhood psoriasis.
Childhood psoriasis is also sometimes misdiagnosed because it is confused with other skin diseases such as atopic or nummular dermatitis, otitis externa, pityriasis rosea, or superficial fungal infections5. Figure 2 details the clinical features of psoriasis to look out for in children of different ages.
Figure 2. Clinical features of paediatric psoriasis by age (adapted from Pinson et al.9).
Find out from Professor Vakirlis more on the challenges of diagnosing childhood psoriasis and the dangers of under- or misdiagnosis.
Triggers
It is worth noting that there are a number of factors that can trigger or exacerbate psoriasis in children. These include environmental and emotional stress, skin trauma (Koebner phenomenon) increased body mass index (BMI), second-hand cigarette smoke, Streptococcus and other infections, Kawasaki disease, withdrawal of systemic corticosteroids, and, tumour necrosis factor (TNF)α inhibitor medications10.
While robust evidence is lacking, Professor Vakirlis describes some of the common environmental factors that can initiate or exacerbate childhood psoriasis.
Disease severity
Defining severity is also more difficult in children. Common measures used in research such as PASI (psoriasis area and severity index) and PGA (physician’s global assessment) haven’t been fully validated in children and severity is not solely related to body surface area (BSA). It also depends on body areas affected and individual perception5,11. For example, scalp psoriasis around the frontal hairline can cause significant impairment in quality of life (QoL) due to its visibility12.
Professor Paller describes how she measures severity in her clinic.
Quality of life
Psoriasis has a large impact on QoL and studies have shown psoriasis to cause one of the greatest QoL impairments among skin diseases13, comparable with other serious paediatric chronic diseases such as arthritis, asthma and diabetes14.
Professor Vakirlis discusses the symptoms that reach beyond the stigma associated beyond physical symptoms.
Patient
The social development domain of the Children’s Dermatology Life Quality Index (CDLQI) shows that children with psoriasis are particularly impaired13 with affected emotional and school functioning15. Unfortunately children often experience teasing, social exclusion by peers, name calling, intimidation, and even in some cases physical violence5. In addition, psoriasis limits recreational activity in at least 15–30% of children with psoriasis16 and the pruritus, sweating, and visible lesions have the greatest detrimental effect on QoL17.
Two aspects rarely considered are the degree of skin scales that children shed and the odour of affected skin. Both are significant problems for many children which add to their embarrassment about their bodies. Dissatisfaction with body image is important to ascertain from patients and asking children to rate their satisfaction with the appearance of their skin on a scale from 1 to 10 is a good way to assess this issue objectively and to validate this concern as being medically important and not just a question of vanity18.
CDLQI
The CDLQI questionnaire has ten questions based on the experiences of children with skin disease over the past week, and has been validated for children aged four to 16 years15. There is also a cartoon version available for the younger children in this age range19 which is popular with both parents and patients. This is available at this external link.
Family
Psoriasis also has a considerable impact on the families of children suffering with the symptoms of the condition. In many cases, parents of affected children may experience the additional emotional burden of having passed psoriasis on to their child20.
Professor Amy Paller describes the tremendous burden of childhood psoriasis on the whole family.
In paediatric patients caregivers have to be involved in disease-related activities, such as doctor visits, and application of treatment(s)21. A study designed to understand parents’ perspectives on young people’s daily life with psoriasis revealed that parents perceived caring for their child as an ongoing stressful learning process having to balance toning down the impact of psoriasis while acknowledging their young people’s needs of multiple treatments and support20.
Another study measured the burden of psoriasis on caregivers and results indicated that psoriasis can be distressing for parents and children alike, disrupting everything from family outings to household activities. Out of 31 parents who participated in the survey, nearly half said they felt sad or frustrated because of their child’s disease. Almost two-thirds of parents reported that they had to change their or their family’s activities to accommodate the needs of their child’s psoriasis22.
Since parental response to any chronic illness can affect the child’s adaptation, interventions such as counselling, stress management and problem solving strategies, will promote better mental health in parents and facilitate better family functioning and care for their children23.
Treating children is very different from adults. We asked Professor Vakirlis about the special challenge of childhood psoriasis and how it can differ between younger children and adolescents.
Comorbidities are often present in childhood psoriasis
Children with psoriasis are at greater risk of obesity, diabetes, anxiety and depression and show marked impairment in emotional, social and school functions24–26.
Professor Vakirlis describes the common comorbidities he sees in his paediatric patients with psoriasis.
Professor Vakirlis describes the common comorbidities he sees in his paediatric patients with psoriasis.
Psoriatic arthritis
While the prevalence of psoriatic arthritis is lower than that in adults affected by psoriasis, there is still an estimated prevalence of 0.7% for all children with psoriasis, rising to 1.2% of patients with psoriasis by 18 years. Indeed, psoriatic arthritis is estimated to account for 6–8% of all inflammatory arthritis cases in children27.
Obesity and metabolic syndrome
While information about the incidence of comorbidities among children with psoriasis is more limited than that in adults, studies have shown increased risk of obesity and cardiovascular risk factors among children with psoriasis compared with those without28,29 (Figure 3).
Figure 3. Increased risk of comorbidities in childhood psoriasis from a German (Augustin et al.28) and US study2 (Paller et al.5).
NS; not significant.
Psychiatric disorders
Studies have also shown that children with psoriasis are also at increased risk for psychiatric disorders and receiving drugs for psychiatric disorders compared with those without29–31.
Figure 4. Increased risk of psychiatric comorbidities in paediatric psoriasis from a Danish (Todberg et al.31) and two US studies (Kimball et al.30; Paller et al.29). % figures are from adjusted hazard ratios and fold changes from incidence rate ratios. ND; not determined; NS, not significant.
Regular screening
Given the recognised link between psoriasis and joint and cardiovascular factors and psychological disorders, guidelines recommend regular screening for children with psoriasis10,26.
- Psoriatic arthritis – routine screening
- Weight – routine assessment for obesity status
- Hypertension – annual screening
- Diabetes –screening every three years
- Depression – routine screening
- Substance abuse – yearly from 11 years
Association of disease severity with comorbidities is unclear. Obesity may be associated with psoriasis severity as it has been shown in one study that a greater number of patients with mild psoriasis were overweight and a greater number of patients with moderate-to-severe psoriasis were obese32. However, a more recent study showed no difference in disease severity with any comorbidity29 and so it is important to be on the lookout for comorbidities even in patients with milder disease.
Treatment data and options are more limited in childhood psoriasis
There are a plethora of treatments available for adults with moderate-to-severe-psoriasis but a lack of efficacy and safety data in paediatric populations means there are far fewer approved treatments available to children and widespread off-label use33.
Topical treatments
Topical treatments are considered first-line therapy in children with mild psoriasis. However, most topical medications are not approved for paediatric use, especially in children under 12 years, and so are extensively used off-label34. Topical treatments included in paediatric guidelines include corticosteroids, calcineurin inhibitors, vitamin D analogues (and various combinations), tazarotene, anthralin and coal tar10.
Professor Paller describes a typical topical treatment regime and why topical treatments are not popular with adolescent patients.
Phototherapy
Phototherapy can be considered as the first-line treatment in patients with more extensive psoriasis and is generally safe and effective in children35. Excimer laser and UVA light with various forms of psoralen (topical, and in some cases oral psoralen plus UVA [PUVA] photochemotherapy) may be used in children with psoriasis and may be efficacious and well tolerated. However, PUVA therapy is contraindicated in children under 12 years because of its related toxicity and probable side effects (nausea, vomiting, photosensitisation and ocular and hepatic toxicity)36.
Phototherapy options have limited supporting evidence and the potential for early skin aging (age spots, wrinkles, loose skin) and increased risk of developing skin cancer needs to be considered36.
Systemic treatments
Systemic treatments of childhood psoriasis can be considered in the case of more severe disease, lack of response to more conservative therapies and impaired physical functioning or QoL10. However, the majority of systemic treatments are not specifically approved for the treatment of psoriasis in children36.
- Methotrexate is effective in the treatment of moderate-to-severe plaque psoriasis, and it is the most prescribed drug for paediatric psoriasis but should be avoided in children for long-term therapy because of cumulative toxicity37
- Ciclosporin A is not approved for childhood psoriasis but it is approved for the prevention of transplant rejection in children above 6 years35
- The retinoid acitretin is effective in paediatric plaque psoriasis, particularly in cases of pustular and erythrodermic disease, but it can take three months of treatment and retinoids are best avoided in young females of childbearing potential because of their teratogenicity36
- Fumaric acid esters (FAE) are used extensively in Germany for psoriasis in adults. There are not many studies on the efficacy of these drugs in children but they may be suitable in cases where methotrexate is contraindicated36
- Apremilast is a phosphodiesterase Type 4 inhibitor approved for use in adults with psoriasis or psoriatic arthritis38. It has been tested in children and phase II results are described in the clinical trials section of the Learning Zone.
Biologic treatments
While there are numerous biologic treatment options for adults with moderate-to-severe psoriasis, the case for approved therapies for paediatric patients is unfortunately different.
Two anti-TNF therapies are approved for use in paediatric patients with moderate-to-severe psoriasis, etanercept39 and adalimumab40. However, there are two other anti-TNF therapies for adults with psoriasis that are not approved for paediatric use in psoriasis. Infliximab is approved for use in children with Crohn’s disease and ulcerative colitis, but not psoriasis41. Certolizumab pegol effectively treats paediatric patients with juvenile idiopathic arthritis with a safety profile similar to other TNF inhibitors but is not approved for paediatric use or being investigated in paediatric trials for psoriasis33.
The IL-12/23 inhibitor ustekinumab is approved for use in paediatric patients with moderate-to-severe psoriasis42 and the IL-17 inhibitor ixekizumab was approved in the US and Europe in 202043,44. More recently, a second IL-17 inhibitor, secukinumab, also received EU approval for the treatment of moderate-to-severe plaque psoriasis in children over six years of age45.
Professor Matthias Augustin, Director of the Institute for Health Services Research in Dermatology and Nursing, in Hamburg, Germany, comments on the benefits and challenges in using IL-17 targeting biologics for paediatric psoriasis.
While a number of clinical trials are ongoing, there is currently a lack of data on the long-term efficacy and safety of biologics in paediatric psoriasis33.
What biologic treatments are currently being investigated for paediatric psoriasis? Professor Matthias Augustin summarises the state of investigational research on biologics for paediatric psoriasis.
What do parents think about biologic treatment for their child? Professor Paller describes the reservations that parents might have and the information that it is important for them to consider in treatment discussions.
References
- Bronckers IMGJ, Paller AS, van Geel MJ, van de Kerkhof PCM, Seyger MMB. Psoriasis in children and adolescents: Diagnosis, management and comorbidities. Pediatric Drugs. 2015;17(5):373–384.
- Burden-Teh E, Thomas KS, Ratib S, Grindlay D, Adaji E, Murphy R. The epidemiology of childhood psoriasis: a scoping review. British Journal of Dermatology. 2016;174(6):1242–1257.
- Paller AS, Singh R, Cloutier M, Gauthier-Loiselle M, Emond B, Guérin A, et al. Prevalence of psoriasis in children and adolescents in the United States: A claims-based analysis. J Drugs Dermatology. 2018;17(2):187–194.
- National Psoriasis Foundation. About Psoriasis in Children. Available at: https://www.psoriasis.org/parents/about-psoriasis. Accessed 11 May 2020.
- Eichenfield LF, Paller AS, Tom WL, Sugarman J, Hebert AA, Friedlander SF, et al. Pediatric psoriasis: Evolving perspectives. Pediatr Dermatol. 2018;35(2):170–181.
- Tollefson MM, Crowson CS, McEvoy MT, Maradit Kremers H. Incidence of psoriasis in children: A population-based study. J Am Acad Dermatol. 2010;62(6):979–987.
- Cordoro KM. Management of childhood psoriasis. Advances in Dermatology. 2008;24(C):125–169.
- Mercy K, Kwasny M, Cordoro KM, Menter A, Tom WL, Korman N, et al. Clinical manifestations of pediatric psoriasis: Results of a multicenter study in the United States. Pediatr Dermatol. 2013;30(4):424–428.
- Pinson R, Sotoodian B, Loretta Fiorillo L. Psoriasis in children. Psoriasis Targets Ther. 2016;Volume 6:121–129.
- Menter A, Cordoro KM, Davis DMR, Kroshinsky D, Paller AS, Armstrong AW, et al. Joint American Academy of Dermatology–National Psoriasis Foundation guidelines of care for the management and treatment of psoriasis in pediatric patients. J Am Acad Dermatol. 2020;82(1):161–201.
- Caroppo F, Zacchino M, Milazzo E, Fontana E, Nobile F, Marogna C, et al. Quality of life in children with psoriasis: results from a monocentric study. G Ital Dermatol Venereol. 2019. doi:10.23736/S0392-0488.19.06368-5.
- Raychaudhuri SK, Maverakis E, Raychaudhuri SP. Diagnosis and classification of psoriasis. Autoimmunity Reviews. 2014;13(4–5):490–495.
- De Jager MEA, Van De Kerkhof PCM, De Jong EMGJ, Seyger MMB. A cross-sectional study using the Childrens Dermatology Life Quality Index (CDLQI) in childhood psoriasis: Negative effect on quality of life and moderate correlation of CDLQI with severity scores. Br J Dermatol. 2010;163(5):1099–1101.
- Beattie PE, Lewis-Jones MS. A comparative study of impairment of quality of life in children with skin disease and children with other chronic childhood diseases. Br J Dermatol. 2006;155(1):145–151.
- Lewis-Jones MS, Finlay AY. The Children’s Dermatology Life Quality Index (CDLQI): initial validation and practical use. Br J Dermatol. 1995;132(6):942–949.
- Gelfand JM, Weinstein R, Porter SB, Neimann AL, Berlin JA, Margolis DJ. Prevalence and treatment of psoriasis in the United Kingdom: A population-based study. Arch Dermatol. 2005;141(12):1537–1541.
- Oostveen AM, De Jager MEA, Van De Kerkhof PCM, Donders ART, De Jong EMGJ, Seyger MMB. The influence of treatments in daily clinical practice on the Children’s Dermatology Life Quality Index in juvenile psoriasis: A longitudinal study from the Child-CAPTURE patient registry. Br J Dermatol. 2012;167(1):145–149.
- Gupta MA, Gupta AK. Evaluation of cutaneous body image dissatisfaction in the dermatology patient. Clinics in Dermatology. 2013;31(1):72–79.
- Holme SA, Man I, Sharpe JL, Dykes PJ, Lewis-Jones MS, Finlay AY. The children’s dermatology life quality index: Validation of the cartoon version. Br J Dermatol. 2003;148(2):285–290.
- Rasmussen GS, Kragballe K, Maindal HT, Lomborg K. Caring for young people with moderate to severe psoriasis: an interpretive description of parental perspectives. J Dermatolog Treat. 2020;31(3):227–234.
- Christin A, Akre C, Berchtold A, Suris JC. Parent-adolescent relationship in youths with a chronic condition. Child Care Health Dev. 2016;42(1):36–41.
- Tollefson MM, Finnie DM, Schoch JJ, Eton DT. Impact of childhood psoriasis on parents of affected children. J Am Acad Dermatol. 2017;76(2):286-289.e5.
- Salman A, Yucelten AD, Sarac E, Saricam MH, Perdahli-Fis N. Impact of psoriasis in the quality of life of children, adolescents and their families: A cross-sectional study. An Bras Dermatol. 2018;93(6):819–823.
- Busch AL, Lieberman AF. Mothers’ adult attachment interview ratings predict preschool children’s iq following domestic violence exposure. Attach Hum Dev. 2010;12(6):505–527.
- de Moll EH, Chang MW, Strober B. Psoriasis in adults and children: Kids are not just little people. Clin Dermatol. 2016;34(6):717–723.
- Osier E, Wang AS, Tollefson MM, Cordoro KM, Daniels SR, Eichenfield A, et al. Pediatric psoriasis comorbidity screening guidelines. JAMA Dermatology. 2017;153(7):698–704.
- Ogdie A, Weiss P. The epidemiology of psoriatic arthritis. Rheumatic Disease Clinics of North America. 2015;41(4):545–568.
- Augustin M, Glaeske G, Radtke MA, Christophers E, Reich K, Schäfer I. Epidemiology and comorbidity of psoriasis in children. Br J Dermatol. 2010;162(3):633–636.
- Paller AS, Schenfeld J, Accortt NA, Kricorian G. A retrospective cohort study to evaluate the development of comorbidities, including psychiatric comorbidities, among a pediatric psoriasis population. Pediatr Dermatol. 2019;36(3):290–297.
- Kimball AB, Wu EQ, Guérin A, Yu AP, Tsaneva M, Gupta SR, et al. Risks of developing psychiatric disorders in pediatric patients with psoriasis. J Am Acad Dermatol. 2012;67(4):651-657.e2.
- Todberg T, Egeberg A, Jensen P, Gislason G, Skov L. Psychiatric comorbidities in children and adolescents with psoriasis: a population-based cohort study. British Journal of Dermatology. 2017;177(2):551–553.
- Paller AS, Mercy K, Kwasny MJ, Choon SE, Cordoro KM, Girolomoni G, et al. Association of pediatric psoriasis severity with excess and central adiposity: An international cross-sectional study. JAMA Dermatology. 2013;149(2):166–176.
- Cline A, Bartos GJ, Strowd LC, Feldman SR. Biologic treatment options for pediatric psoriasis and atopic dermatitis. Children. 2019;6(9):103.
- Bhutani T, Kamangar F, Cordoro KM. Management of pediatric psoriasis. Pediatr Ann. 2012;41(1):e1-7.
- Relvas M, Torres T. Pediatric psoriasis. American Journal of Clinical Dermatology. 2017;18(6):797–811.
- D’Adamio S, Silvaggio D, Massaro A, Lombardo P, Bianchi L, Talamonti M, et al. Pharmacotherapeutic management of psoriasis in adolescents and children. Expert Opin Pharmacother. 2019;20(14):1777–1785.
- Mahé E. Childhood psoriasis. European Journal of Dermatology. 2016;26(6):537–548.
- Otezla 10 mg Film-coated Tablets - Summary of Product Characteristics (SmPC). Available at: https://www.medicines.org.uk/emc/product/10709/smpc. Accessed 14 May 2020.
- Enbrel 10 mg powder and solvent for solution for injection for paediatric use - Summary of Product Characteristics (SmPC). Available at: https://www.medicines.org.uk/emc/product/4677/smpc. Accessed 14 May 2020.
- Humira 20 mg / 0.2 ml Solution for Injection in Pre-Filled Syringe - Summary of Product Characteristics (SmPC). Available at: https://www.medicines.org.uk/emc/product/9080/smpc. Accessed 14 May 2020.
- Remicade 100mg powder for concentrate for solution for infusion - Summary of Product Characteristics (SmPC). Available at: https://www.medicines.org.uk/emc/product/3831. Accessed 14 May 2020.
- Stelara 45 mg solution for injection (vials) - Summary of Product Characteristics (SmPC). Available at: https://www.medicines.org.uk/emc/product/4413/smpc. Accessed 22 June 2020.
- Lilly Presents Positive Results for Taltz® (ixekizumab) in Pediatric Patients with Moderate to Severe Plaque Psoriasis at the 28th Annual European Academy of Dermatology and Venereology (EADV) Congress. https://investor.lilly.com/news-releases/news-release-details/lilly-presents-positive-results-taltzr-ixekizumab-pediatric. Accessed 9 March 2020.
- Taltz 80 mg solution for injection in pre-filled syringe - Summary of Product Characteristics (SmPC). Available at: https://www.medicines.org.uk/emc/product/7233/smpc. Accessed 13 January 2021.
- European Medicines Agency. Cosentyx: Pending EC decision. Available at: https://www.ema.europa.eu/en/medicines/human/summaries-opinion/cosentyx-0. Accessed 2 July 2020.
of interest
are looking at
saved
next event
This content has been developed independently by Medthority who previously received educational funding in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content.
