Welcome
What Is Type 2 Inflammation?
Type 2 inflammation is a common driver for underlying pathophysiology across multiple inflammatory diseases, including eosinophilic esophagitis (EoE). EoE is a chronic, progressive type 2 inflammatory disease characterized by symptoms of esophageal dysfunction and eosinophilic infiltration of the esophageal mucosa in the absence of secondary causes of eosinophilia1,2
Involving both the adaptive and innate arms of the immune system, type 2 inflammation is characterized by key cytokines, particularly interleukin (IL)-5, IL-4, and IL-13 (FIGURE 1).1-9
FIGURE 1. Type 2 Inflammation Is Driven by Both the Adaptive and Innate Arms of the Immune System.3-8
*Downstream from Th2 cells, innate cells (such as mast cells and basophils) can also play a role in adaptive immunity given their activation by antigen-bound IgE. Crosslinking of IgE on these cells leads to release of several inflammatory mediators, thus amplifying the type 2 inflammatory response.1
†These cell types also produce IL-31, which is associated with some inflammatory diseases of the skin.8
IgE, immunoglobulin E; ILC2, type 2 innate lymphoid cell; Th2, T helper type 2.
Underlying type 2 inflammation plays a role across multiple diseases in a range of organ systems (FIGURE 2).3,9-20
FIGURE 2. Type 2 Inflammation Plays a Role Across Multiple Diseases.3,9-20
AFRS, allergic fungal rhinosinusitis; COPD, chronic obstructive pulmonary disease; CRSsNP, chronic rhinosinusitis without nasal polyps; IL, interleukin; NSAID-ERD/AERD, nonsteroidal anti-inflammatory drug-exacerbated respiratory disease/aspirin-exacerbated respiratory disease.
Burden of Disease
Type 2 inflammatory diseases, including eosinophilic esophagitis, are associated with substantial disease-specific signs, symptoms, and impaired quality of life (FIGURE 3).14,21-23
FIGURE 3. Common Aspects of Diseases Mediated by Type 2 Inflammation. 14,21-23
CRSwNP, chronic rhinosinusitis with nasal polyps.
Pathophysiology
Eosinophilic esophagitis shares a common underlying pathophysiology with other type 2 inflammatory diseases.3
Type 2 Inflammation: Pathophysiologic Features That Underlie Multiple Inflammatory Diseases
Watch this short video to learn about the common pathophysiology underlying type 2 inflammatory diseases, including eosinophilic esophagitis. Clinical manifestations from this shared pathophysiology and the additional burden from coexisting type 2 inflammatory diseases are also presented, supporting the important role of type 2 inflammation across multiple diseases.
IL-4 and IL-13 are key and central drivers of systemic and local tissue inflammation and mediate different pathophysiologic consequences across type 2 inflammatory diseases (FIGURE 4).3,14,21,23-28
FIGURE 4. IL-4 and IL-13 Are Key and Central Drivers of Systemic and Local Tissue Inflammation.3,14,21,23-28
CRSwNP, chronic rhinosinusitis with nasal polyps; IL, interleukin.
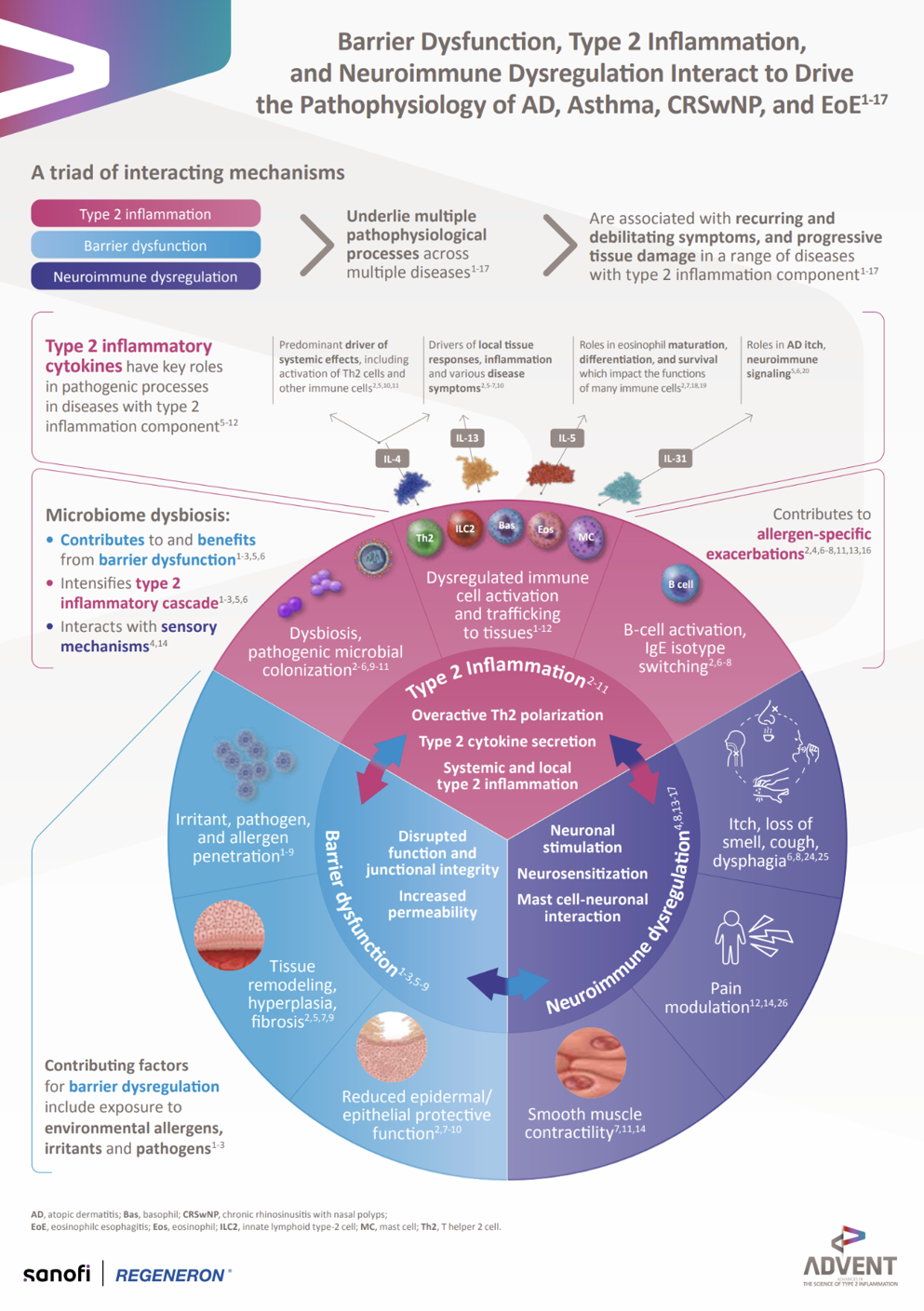
Type 2 Inflammation, Barrier Dysfunction, and Neuroimmune Dysregulation Infographic
Learn how type 2 inflammation, barrier dysfunction, and neuroimmune dysregulation interact to drive the pathophysiology of EoE and other diseases.
Download: Type 2 Inflammation, Barrier Dysfunction, and Neuroimmune Dysregulation Infographic
Identifying Type 2 Inflammation
EoE is diagnosed on the basis of symptoms of esophageal dysfunction and eosinophilic inflammation of the esophagus, with at least 15 eos/hpf in esophageal mucosal biopsy specimens and exclusion of other causes of esophageal eosinophilia (such as celiac disease or Crohn’s disease with eosinophilic-predominant esophageal inflammation). EoE pathophysiology is not solely mediated by eosinophils; other type 2 inflammatory cells and cytokines play an important role (FIGURE 5).1,2,29,30
FIGURE 5. EoE Pathophysiology Is Not Solely Mediated by Eosinophils.1,2,29,30
*Eosinophil activation and recruitment to the esophagus in EoE are mediated by key type 2 cytokines (IL-4, IL-13, IL-5)
EoE, eosinophilic esophagitis; eos/hpf, eosinophils per high-powered field; IL, interleukin; ILC2, type 2 innate lymphoid cell; TGF-β, transforming growth factor beta; Th2, T helper type 2.
Recognizing features of type 2 inflammation plays an important role in identification and diagnosis of diseases such as eosinophilic esophagitis, predominantly driven by type 2 inflammation (FIGURE 6).2,26,31-35
FIGURE 6. IL-4 and IL-13 Are Key and Central Drivers of Type 2 Pathophysiology in EoE. 2,26,31-35
IL, interleukin; ILC2, innate lymphoid cell type 2; QoL, quality of life; Th2, T helper 2; TSLP, thymic stromal lymphopoietin.
References
- Hirano I, et al. Gastroenterology. 2020;158(6):1776-1786.
- Lucendo AJ, et al. United European Gastroenterol J. 2017;5(3):335-358.
- Gandhi NA, et al. Nat Rev Drug Discov. 2016;15(1):35-50.
- Ahern S, et al. Medicina (Kaunas). 2019;55(4):95.
- Kim DW, et al. Allergy Asthma Immunol Res. 2017;9(4):299-306.
- Kariya S, et al. Advan Cell Molec Otolaryngol. 2015;3(1):26601.
- Gandhi NA, et al. Expert Rev Clin Immunol. 2017;13(5):425-437.
- Mahdavinia M, et al. J Allergy Clin Immunol. 2014;133(6):1759-1763.
- Stott B, et al. J Allergy Clin Immunol. 2013;132(2):446-454.e5.
- Fukushi S, et al. Br J Derm. 2011;165(5):990-996.
- Teraki Y, et al. J Invest Dermatol. 2001;117(5):1097-1102.
- Chehade M, et al. Gastro Hep Advances. 2022;1(5):720-732.
- Bachert C, et al. World Allergy Organ J. 2014;7(1):25.
- Schleimer RP. Annu Rev Pathol. 2017;12:331-357.
- Stevens WW, et al. J Allergy Clin Immunol Pract. 2019;7(8):2812-2820.
- Cho SH, et al. J Allergy Clin Immunol Pract. 2020;8(5):1505-1511.
- Kowalski ML, et al. Curr Opin Pulm Med. 2019;25(1):64-70.
- Garudadri S, Woodruff PG. Ann Am Thorac Soc. 2018;15(suppl 4):S234-S238.
- Rathore VP, et al. Clin Immunol. 2001;100(2):228-235.
- Kurup VP, et al. J Allergy Clin Immunol. 1994;93(6):1013-1020.
- Weidinger S, Novak N. Lancet. 2016;387(10023):1109-1122.
- Hill DA, Spergel JM. Curr Allergy Asthma Rep. 2016;16(2):9.
- Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention. Updated July 2022. Accessed October 16, 2022. https://ginasthma.org/reports/
- Nguyen JK, et al. Arch Dermatol Res. 2020;312(2):81-92.
- Langan SM, et al. Lancet. 2020;396(10247):345-360.
- Davis BP, Rothenberg ME. Annu Rev Pathol. 2016;11:365-393.
- Weigelt N, et al. J Cutan Pathol. 2010;37(5):578-586.
- Pereira MP, et al. J Eur Acad Dermatol Venerol. 2018;32(7):1059-1065.
- Dellon ES, et al. Gastroenterology. 2018;155(4):1022-1033.
- Chehade M, et al. Gastro Hep Advances. 2022;1(5):720-732.
- Caldwell JM, et al. Curr Opin Immunol. 2017;48:114-121.
- Davis BP. Clin Rev Allergy Immunol. 2018;55(1):19-42.
- Wechsler JB, Bryce PJ. Gastroenterol Clin North Am. 2014;43(2):281-296.
- Dellon ES, Hirano I. Gastroenterology. 2018;154(2):319-332.e3.
- Safroneeva E, et al. Aliment Pharmacol Ther. 2015;42(8):1000-1010.
of interest
are looking at
saved
next event
Developed by EPG Health for Medthority in collaboration with Sanofi and Regeneron, with content provided by Sanofi and Regeneron.
ADVENT is a medical education non-promotional program for healthcare professionals organized by Sanofi and Regeneron. This website is intended only for duly authenticated healthcare professionals.
© 2024 Sanofi and Regeneron Pharmaceuticals, Inc. All Rights Reserved.
MAT-US-2209565 v2.0 - P Expiration Date: 01/17/2025
Sanofi and Regeneron are committed to providing resources to advance knowledge in areas of unmet medical need among patients with inflammatory and immunologic diseases.